January 2025
Arthritis Can Cause Pain in the Feet and Ankles
Causes and Symptoms of Diabetic Foot Wounds

Diabetic foot wounds develop from a combination of nerve and blood vessel damage caused by prolonged high blood sugar levels. Nerve damage, or neuropathy, reduces sensation in the feet, making it difficult to notice minor injuries like cuts or blisters. Also, poor blood flow, resulting from damaged blood vessels, slows healing and increases the risk of infections. Common triggers for diabetic foot wounds include wearing ill-fitting shoes, foot deformities like bunions or hammer toes, and excessive callus formation. Early symptoms may include dry or warm skin, tingling, and numbness. The appearance of poorly healing sores, particularly on the soles, toes, or heels are other factors. In advanced cases, such wounds can deepen, become infected, or result in tissue death and possible limb loss. A podiatrist can assess nerve and blood flow issues, treat wounds, and recommend preventive measures like proper footwear and regular foot examinations. If you have foot problems related to diabetes, it is suggested that you schedule an appointment with a podiatrist for ongoing foot care.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Coastal Foot & Ankle Wellness Center, LLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Care for Diabetic Foot
Millions of people are affected by diabetes each year. Diabetes damages blood vessels in all parts of the body, especially the feet. The legs and feet may develop slow blood flow, which causes neuropathy, or nerve damage. Once a diabetic patient develops neuropathy, it is important that the feet are well taken care of. Otherwise, the lower limbs may have to be amputated. This only happens in drastic cases, but it shows how seriously diabetic foot care should be taken.
It is very important to always wash and dry the feet thoroughly, especially in between the toes, if you’re a diabetic. Secondly, examining your feet and toes for redness or sores must be done, even if you do not feel pain. You may also want to examine your feet from the bottom. Try to avoid wearing colored socks to prevent infections that may occur from the dye. Well-fitting socks are also highly recommended.
A diabetic’s physician should always monitor their blood levels to test how well blood sugars are being maintained. In addition to giving advice about everyday eating habits and foot care, a physician may prescribe medicine to help with the diabetic patient’s neuropathy. It is also advised to see a podiatrist if experiencing any feet conditions. Toenails may also need to be taken care of by a podiatrist. This prevents patients from cutting too deeply around their cuticles, which can lead to infection.
A person can take care of their feet at home by following the instructions of their physician. Using creams on one’s feet is also an effective way to heal dryness. Proceed with caution when using tools to remove calluses, as severe diabetics may not be able to feel pain on their feet. If any complications arise do not hesitate to contact a podiatrist.
On a daily basis, diabetic feet must be checked. If you are ever concerned about something, contact your health care professional. You never want to wait until a wound becomes too severe to treat. If left untreated, gangrene may develop. Gangrene is a serious infection that can lead to sepsis or amputation. It is also important for diabetics to be on the lookout for ulcers. Ulcers are sores that develop from tissue loss on the skin. They can be quite painful and require intensive treatment. Early treatment and everyday inspection are imperative to staying healthy.
Managing Ingrown Toenails

Ingrown toenails, commonly affecting the big toe, occur when the edge of the nail grows into the surrounding skin, causing pain, redness, and swelling. In some cases, infection can develop, leading to increased discomfort and drainage. The condition can result from improper nail trimming, wearing tight shoes, or injury to the toe. Certain foot shapes or conditions, like curved nails, can also contribute. Symptoms include throbbing pain, swelling around the nail, and sometimes pus if infection is present. Relief options vary depending on the severity. In mild cases, soaking the foot, wearing comfortable shoes, and carefully trimming the nail may offer relief. For more severe cases, a podiatrist might remove part of the nail or prescribe antibiotics if an infection is present. In recurring cases, permanent nail removal may be considered. If you have developed an ingrown toenail, it is suggested that you schedule an appointment with a podiatrist.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact one of our podiatrists of Coastal Foot & Ankle Wellness Center, LLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ingrown Toenail Care
An ingrown toenail is a nail that has curved downward and grows into the skin. This typically occurs at the nail borders, or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. Milder cases that don’t involve infection or other medical conditions can benefit from soaking the feet in room-temperature water and gently massaging the side of the nail. In most cases, however, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Tips for Preventing Falls in Seniors

Falls are a common risk among seniors and can lead to serious injuries, including fractures and hospitalization. Foot problems, such as weakness in the ankles, instability in the toes, or wearing improper footwear, significantly increase the likelihood of falls. Falls among seniors can often result from reduced foot strength or balance issues that stem from conditions like arthritis or neuropathy. A podiatrist can play a vital role in preventing falls in this age group by addressing foot-related concerns. This foot doctor can evaluate gait and recommend proper footwear that provides better grip and support. A podiatrist also can treat or manage other conditions that affect stability, such as corns, bunions, or poorly fitted orthotics. Regular checkups can help identify problems early, improve mobility and reduce the risk of falling. Maintaining strong, stable feet and ankles is essential for safety and independence among seniors. If you are a senior at risk of falling, it is suggested that you schedule an appointment with a podiatrist for guidance.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with one of our podiatrists from Coastal Foot & Ankle Wellness Center, LLC. Our doctors will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Understanding Morton's Neuroma
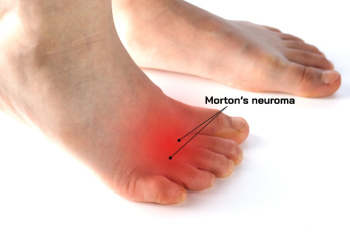
Morton’s neuroma is a painful condition affecting the ball of the foot, often between the third and fourth toes. It occurs when the tissue surrounding a nerve becomes thickened, causing pain, burning, or a sensation of something being wedged in the shoe. The pain can worsen when walking, standing, or wearing tight shoes. The primary cause of Morton’s neuroma is excessive pressure or irritation on the nerve, often from wearing high heels, tight shoes, or engaging in repetitive activities like running. Foot deformities, such as bunions or hammertoes, can also increase the risk. A podiatrist can help diagnose Morton’s neuroma through a physical exam and imaging tests. Treatments may include wearing custom orthotics, padding, or shoe modifications to reduce pressure on the affected area. In more severe cases, corticosteroid injections or even surgery may be recommended. If you have pain in this part of your foot, it is suggested that you schedule an appointment with a podiatrist.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Coastal Foot & Ankle Wellness Center, LLC. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.








