Tarsal Tunnel Syndrome Causes
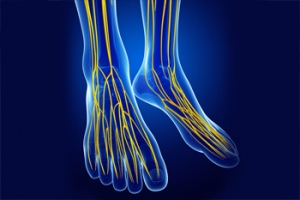
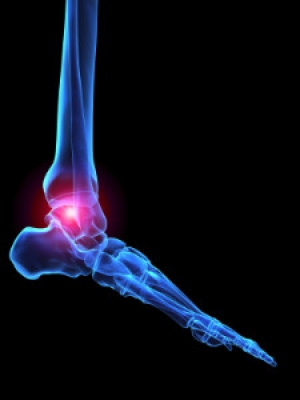
The tarsal tunnel is a narrow space in the inner ankle that has nerves, blood vessels, and tendons passing through it. When the posterior tibial nerve inside of the tarsal tunnel is compressed, this leads to a painful condition called tarsal tunnel syndrome. Symptoms of this condition include foot pain, a pins and needles sensation, numbness, and swelling. The nerve compression that brings about tarsal tunnel syndrome can be caused by sports injuries, lesions, such as ganglion cysts, that occupy space in the tunnel, excess fluid buildup, changes in the biomechanics of the foot, wearing tight, ill-fitting shoes, or other medical conditions like diabetes and arthritis. In about 30% of cases, the cause is unknown. Nevertheless, tarsal tunnel syndrome can be treated and usually resolves within several weeks of treatment. If you have symptoms of this condition, please seek the care of a podiatrist.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact one of our podiatrists of Coastal Foot & Ankle Wellness Center, LLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treating Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which the tibial nerve, located in the tarsal tunnel in the foot, is compressed. The tibial nerve can become compressed from injury, such as an ankle sprain, flat feet, and lesions. Arthritis, diabetes, and varicose veins can also cause swelling and thus result in nerve compression.
Symptoms of tarsal tunnel syndrome include several different sensations in the sole of the foot, inside the ankle, and around the tibial nerve. These sensations include shooting pains, numbness or reduced sensation, pins and needles, burning, and tingling. Symptoms tend to worsen with greater activity to the area. In rare and severe occasions, this can change the muscles in the foot.
If you suspect you have tarsal tunnel syndrome, you should consult with your podiatrist. He or she will examine your medical history to see if you have a history of diabetes, arthritis, or flat feet. They will also check to see if you have suffered an injury to the area recently. An electrical test will be conducted to check if the nerve has been damaged. A simpler Tinel’s Test might also be used. This includes simply tapping the nerve to create a sensation. An MRI scan of the area may also be used.
Treatments vary greatly for tarsal tunnel syndrome. Treatments include both nonsurgical and surgical options depending upon the severity of the condition. Nonsurgical options include anti-inflammatory medication and steroid injections to the area. Orthotics, such as a splint or brace that immobilizes the foot, is another noninvasive option. For those with flat feet, custom shoes can be made to offer better foot support. Surgical options include a tunnel tarsal release, in which an incision is made behind the ankle down to the arch of the foot. This releases the ligament and relieves pressure off the nerve. Some doctors use a more minimally invasive surgery, where smaller incisions are made in the ankle and the ligament is stretched out.
If you are suffering from painful sensations in your foot, see a podiatrist who can determine if you are experiencing tarsal tunnel syndrome. Tarsal tunnel syndrome that is left unchecked can cause permanent nerve damage to the foot.
Why Live with Pain and Numbness in Your Feet?
Obesity and the Feet in Older Adults
Obesity affects every part of your body - including your feet and ankles. People over 60 who are obese have been found to experience more foot pain, have reduced toe and ankle strength, and have a slower walking speed, among other problems. Excess body weight strains the lower limbs, leading to functional and structural changes that can impact your mobility and quality of life. This is particularly the case for older adults. One of the best ways to maintain the health of your feet and improve your overall health is to eat a healthy diet, exercise, and lose weight. Unfortunately, this can be very difficult if you have foot and ankle pain that makes it harder to exercise or even stand for long periods of time. A podiatrist can help you reduce foot and ankle pain and increase your mobility so that you can improve your quality of life. For more information, please consult with a podiatrist.
The more you weigh, the harder your feet must work to support your body. If you’re an obese individual and are concerned about your feet, contact one of our podiatrists from Coastal Foot & Ankle Wellness Center, LLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Obesity and Your Feet
People who are overweight are putting more pressure on their ankles, knees, and hips as well as their feet. This unfortunately can lead to variety of different issues.
Problems & Complications Stemming from Obesity
- When the body is overweight, it tries to compensate by changing the way that it moves. An obese person may lean forward and put extra weight on the wrong part of the foot. This puts unnecessary stress on the feet.
- Obese people are also more likely to develop type II diabetes which is a condition that causes a lot of foot problems. People with diabetes often don’t feel the cuts and sores that they may have on their feet, which can lead to more complicated and severe issues.
- Plantar fasciitis is another foot condition that can be caused by obesity. Plantar fasciitis is an inflammation of the tissue along the bottom of the foot, which causes pain and stiffness while walking and climbing stairs.
If you have any questions, please feel free to contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How Obesity Affects Your Feet
Gaining weight can happen suddenly and at any time. Usually you won’t notice the extra weight until your feet start hurting at the end of the day. This happens as your feet begin adjusting to carrying more weight. Foot swelling and pain are two of the biggest side effects of having gained weight.
Many foot-related problems can occur even after just putting on a few pounds. This includes the body ‘compensating’ by changing the way it moves. You may find yourself putting extra weight on the wrong parts of your feet and even leaning forward a bit. Your feet were designed to carry a healthy, normal body weight. Extra weight places undue stress on them.
Being overweight often causes the development of Type-2 diabetes, causing leg and foot pain. Older people who do not attempt to control their condition can even lose sensation and feeling in their legs and feet. This can lead to the development of small sores that can lead to serious infection.
Extra stress placed on the joints, tendons and muscles in the feet as a result of extra body weight may also cause heel spurs, or plantar fasciitis. Plantar fasciitis is an inflammation of the foot tissue, causing stiffness and pain when walking and climbing stairs. This can usually be relieved by foot stretches and custom made orthotic shoe-inserts.
Problems in the feet triggered by obesity can be treated by paying special attention to footwear. Proper support shoes that allow for good circulation, especially in the arch and ankle, are vital. A podiatrist can help you find what sort of shoe is most suitable for your feet. They can also measure you for special orthotics if necessary.
It could also be high time to start losing weight in order to treat and prevent diabetes as well as other life threatening diseases. Some methods include yoga and water aerobics, which benefit your entire body without placing stress on your feet. Don’t risk losing your feet by losing interest in them. Take care of your feet and your body, as they deserve the very best.
What Is Infectious Arthritis?
 Infectious arthritis is a sudden and painful form of arthritis caused by bacterial, viral, or fungal infections. This type of arthritis typically only affects one joint and can be caused by an infection spreading from one part of your body to the joint or joint lining, or by an infection-causing germ entering the body through open wounds, injections, or surgery. The symptoms of infectious arthritis include intense swelling, pain, fever, and chills. Although infectious arthritis usually affects the knees, it can also attack hips, wrists, and ankles. If you have symptoms of infectious arthritis in your ankle, a podiatrist may be able to help. For more information about the different types of arthritis, the effects of arthritis on your feet, and how to care for arthritic feet and ankles, please consult with a podiatrist.
Infectious arthritis is a sudden and painful form of arthritis caused by bacterial, viral, or fungal infections. This type of arthritis typically only affects one joint and can be caused by an infection spreading from one part of your body to the joint or joint lining, or by an infection-causing germ entering the body through open wounds, injections, or surgery. The symptoms of infectious arthritis include intense swelling, pain, fever, and chills. Although infectious arthritis usually affects the knees, it can also attack hips, wrists, and ankles. If you have symptoms of infectious arthritis in your ankle, a podiatrist may be able to help. For more information about the different types of arthritis, the effects of arthritis on your feet, and how to care for arthritic feet and ankles, please consult with a podiatrist.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact one of our podiatrists from Coastal Foot & Ankle Wellness Center, LLC. Our doctors can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Care for Your Arthritic Foot
Arthritis is an inflammation of the joints and it can occur at any joint in the body, especially in the foot. It generally effects those who are older, however, it can occur at any age. Although there are many different forms of arthritis, there are three main types that occur in the foot. The three types are osteoarthritis, rheumatoid arthritis, and gout.
The primary cause of osteoarthritis is aging. As you age, cartilage degenerates around the joints which causes friction and pain. Obesity can cause osteoarthritis through mechanical stress. Injuries that damage joints can increase the probability as well. Finally, a family history of osteoarthritis can also increase chances of having it.
Rheumatoid arthritis occurs when the immune system attacks the joint linings and weakens them over a long time. While there is no known cause of rheumatoid arthritis, obesity and smoking can increase your chances of getting it. Women are also more likely to get it than men.
Gout is a form of arthritis that occurs when there is too much uric acid in your blood and painful crystals form in your joints. Men are more likely to have gout than women. People who are obese or drink alcohol often are also more likely to develop gout. Furthermore, having diabetes, heart disease, high blood pressure, high cholesterol, gastric bypass surgery or a family history of gout may increase your likelihood of developing the condition.
Symptoms of arthritis include pain, stiffness, swelling in the joints. These symptoms can make it harder and more painful to walk. Physical activity can increase pain and discomfort. Furthermore, joint pain can worsen throughout the day for osteoarthritis. Gout attacks generally last several days with the first few being the worst.
Diagnosis of gout includes either a joint fluid test or a blood test. X-ray imaging can detect osteoarthritis but not gout. On the other hand, there is no blood test for osteoarthritis. Rheumatoid arthritis is difficult to diagnosis. Doctors utilize family and personal medical history, a physical examination, and antibody blood tests to determine if you have rheumatoid arthritis.
Treatment varies for the different kinds of arthritis. Anti-inflammatory medication or steroids can help reduce pain from inflammation of the joints. Changing shoe types can help with some symptoms. Wider shoes can help with discomfort from gout and osteoarthritis. High heels should be avoided. Shoes with proper arch support and that take pressure off the ball of the foot can help with rheumatoid arthritis. Drinking lots of water can also help rid uric acid from the blood. Losing weight, improving your diet, and limiting alcohol and smoking can also help prevent or lessen the symptoms of arthritis.
If you are having trouble walking or pain in your feet, see a podiatrist to check if you have arthritis.
Understanding Warts on the Feet
 A verruca is a small wart on the sole of the foot. They are more commonly known as plantar warts. Plantar warts can grow on the sole of the foot because of the human papillomavirus (HPV). This virus is contagious and thrives in warm and moist environments like locker rooms and swimming pools which makes plantar warts common for people who are barefoot in these communal areas. Plantar warts are not usually painful unless they are bearing weight. Some patients have found they may be tender to the touch as well. To avoid the spread of plantar warts, you should wear flip flops in communal areas such as pools, locker rooms, or showers. If you have a plantar wart that persists, consulting with a podiatrist and getting professional advice can be extremely beneficial.
A verruca is a small wart on the sole of the foot. They are more commonly known as plantar warts. Plantar warts can grow on the sole of the foot because of the human papillomavirus (HPV). This virus is contagious and thrives in warm and moist environments like locker rooms and swimming pools which makes plantar warts common for people who are barefoot in these communal areas. Plantar warts are not usually painful unless they are bearing weight. Some patients have found they may be tender to the touch as well. To avoid the spread of plantar warts, you should wear flip flops in communal areas such as pools, locker rooms, or showers. If you have a plantar wart that persists, consulting with a podiatrist and getting professional advice can be extremely beneficial.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from Coastal Foot & Ankle Wellness Center, LLC. Our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
All About Plantar Warts
Plantar warts are warts that are only found on the feet, hence the term “plantar”, which means “relating to the foot.” They are caused by the human papillomavirus, or HPV, and occur when this virus gets into open wounds on the feet. The warts themselves are hard bumps on the foot. They are easily recognizable, mostly found on the heels or ball of the foot. Plantar warts are non-malignant, but they can cause some pain, discomfort, and are often unsightly. Removing them is a common step toward treating them.
Plantar warts can cause some pain while standing, sometimes felt as tenderness on the sole of your foot. Unless the wart has grown into the foot behind a callus, you will be able to see the fleshy wart. A podiatrist should only be consulted if there is an excessive amount of pain. Plantar warts are not cancerous or dangerous, but they can affect your walking and continually reappear. Anyone who suffers from diabetes or a compromised immune system disease should seek out care immediately.
Podiatrists are easily able to diagnose plantar warts. They usually scrape off a tiny bit of the rough skin to make tiny blood clots visible and examine the inside of warts. However, a biopsy can be done if the doctor is not able to diagnose them from simply looking at them. Although plantar warts usually do not require an excessive amount of treatment, there are ways to go about removing them. A common method is to freeze them off using liquid nitrogen, removing them using an electrical tool, or burning them off via laser treatment. For a less invasive treatment option, topical creams can be used through a doctor’s prescription. This treatment method takes more time, however. Keep the wart covered for protection in between daily treatments.
The best way to avoid developing plantar warts is to avoid walking barefoot in public places. Avoid this especially if you have open sores or cuts on your feet. It is also important to avoid direct contact with warts in general, as they are highly contagious.
Foot Pain and Walking
 Foot pain may become worse while walking. Many patients experience occasional aches and pains in their feet, and chronic pain may indicate serious or underlying foot conditions. Pain in the heel may represent plantar fasciitis, which is an inflammation of the plantar fascia. This is the portion of tissue that connects the heel to the toes, and may feel worse upon arising in the morning. A condition that affects the nerves in the foot may indicate Morton’s neuroma, and the pain is often felt in the ball of the foot. In severe cases, it may gravitate to the toes, which can cause the entire foot to feel uncomfortable. There are several types of tendinitis that can cause severe pain. When the Achilles tendon is affected, the heel and calf are targeted. Extensor tendonitis can cause the top of the foot pain and discomfort, and the outside and back of the foot can be affected by peroneal tendonitis. Any type of foot pain warrants a visit to the podiatrist, who can properly diagnose and treat painful foot conditions.
Foot pain may become worse while walking. Many patients experience occasional aches and pains in their feet, and chronic pain may indicate serious or underlying foot conditions. Pain in the heel may represent plantar fasciitis, which is an inflammation of the plantar fascia. This is the portion of tissue that connects the heel to the toes, and may feel worse upon arising in the morning. A condition that affects the nerves in the foot may indicate Morton’s neuroma, and the pain is often felt in the ball of the foot. In severe cases, it may gravitate to the toes, which can cause the entire foot to feel uncomfortable. There are several types of tendinitis that can cause severe pain. When the Achilles tendon is affected, the heel and calf are targeted. Extensor tendonitis can cause the top of the foot pain and discomfort, and the outside and back of the foot can be affected by peroneal tendonitis. Any type of foot pain warrants a visit to the podiatrist, who can properly diagnose and treat painful foot conditions.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from Coastal Foot & Ankle Wellness Center, LLC. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact one of our offices located in St. Augustine, and Palatka, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.